Anal Fistula - Types, Causes, And Symptoms
A fistula is a tiny channel left behind after pus has drained. There are some chronic intestinal disorders that have been linked to the development of an anal fistula.
Author:Daniel JamesReviewer:Karan EmeryJan 19, 202311.9K Shares746.5K Views

An abscess forms when pus from an infection in the area of your anus drains into the space between your intestines. This results in a fistula forming in your anus.
A fistula is a tiny channel left behind after pus has drained. There are some chronic intestinal disorders that have been linked to the development of an anal fistula.
Definition Of Anal Fistula
An infected cavity in the anus, which is called an abscess, and a hole on the skin surrounding the anus are connected by a short tunnel called an anal fistula. The external passage through which the body excretes feces is called the anus.
Numerous tiny glands that produce mucus are located right inside the anus. These glands can sometimes become congested and infected, which can result in an abscess. These abscesses have a 50/50 chance of turning into fistulas.
What is Anal Fistula | Different Types of Anal Fistula | 0806-5417-722
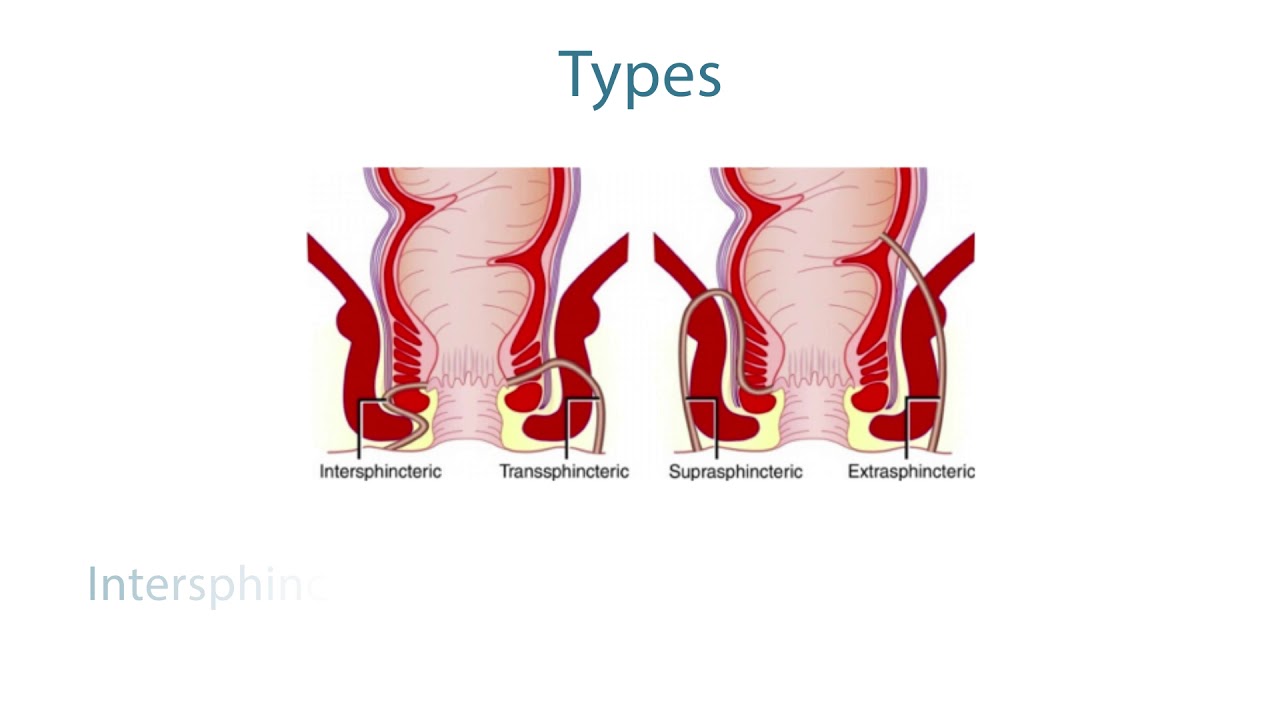
Types Of Anal Fistula
In terms of the degree of seriousness, anal fistulas can be divided into two categories: the simple fistula and the complex fistula.
- A simple fistula is characterized by a single opening tract that extends from the anus to the skin and minimal interaction of the external anal sphincters, a layer of voluntary muscle that lines the outside wall of the anal canal and anal opening.
- Multiple tracts linking the anus to the skin or nearby organs are the most common presentation of complex fistula. The external sphincter is severely compromised by complex fistulas, which can result in fecal incontinence.
Causes Of Anal Fistula
There are multiple fluid-producing glands right inside your anus. They occasionally become obstructed or clogged. When that takes place, an accumulation of germs may enlarge a pocket of contaminated tissue and fluids. This is referred to as an abscess.
It will spread if the abscess is not treated, and will inevitably get outside and pierce the skin close to the anus to allow the goop within to drip. The channel that joins the gland to that hole is known as a fistula.
An abscess typically results in a fistula. It's uncommon, but they can arise as a result of diseases like tuberculosis, sexually transmitted diseases (STDs), or chronic bowel diseases like Crohn's disease or ulcerative colitis.
Symptoms Of Anal Fistula
Anal fistulas can produce uncomfortable symptoms including soreness and skin irritability, and they typically don't go away on their own. Anal fistula symptoms can include the following:
- Irritation of the skin close to the anus.
- A pounding discomfort that is constant. You might have a worsening of the pain when you sit down, when you walk about, when you cough, or when you poop.
- A putrid discharge coming from the area next to your anus.
- Having bloody or pus-filled stools when you poop.
- Difficulty controlling bowel movements.
There is a possibility that an abscess can form, which will result in fever, redness, and swelling in the area around your anus.

What is an Anal Fistula
Tests For Anal Fistula
You should make an appointment with your primary care physician if you have symptoms that continue to indicate that you may have an anal fistula. Your anus will be examined, and your doctor will carefully place their finger into your back passageway (a procedure known as a rectal examination) to look for any indications of a fistula.
If your primary care physician suspects that you have a fistula, they will send you to a bowel specialist for additional testing to confirm the diagnosis and choose the therapy that will be most effective in your case. These testing might involve the following:
- Proctoscopy:To inspect the anus, a light-equipped telescope is employed.
- An ultrasound scan, magnetic resonance imaging (MRI), or computerised tomography (CT) scan.
Treatments For Anal Fistula
The location, severity, and underlying etiology of an anal fistula all have a role in how it is treated. Total anal fistula repair is sought after for the sake of sphincter muscle health and the prevention of a recurrence. A loss of control over bowel movements is a possible complication of damage to these muscles. Though surgery is typically necessary, non-invasive options may be available in rare cases.
Among the available surgical options are:
- Endorectal advancement flap:In order to close the fistula, the surgeon first makes a flap in the rectal wall. In order to hide the patches, the flap is used. The quantity of sphincter muscle that is removed during this process can be minimized.
- Fistulotomy.The surgeon cuts the fistula's internal opening, scrapes and flushes contaminated tissue, flattens the tunnel, and sutures it. A complex fistula may require tunnel removal by the surgeon. If the tunnel isn't located or a lot of sphincter muscle must be severed, fistulotomy may be done in two stages.
- Ligation of the intersphincteric fistula tract (LIFT).For deeper fistulas, LIFT is a two-step treatment. The LIFT method lets the surgeon access the fistula without cutting the sphincter muscles. A silk or latex seton is placed into the fistula tunnel first. The tunnel progressively expands. After a few weeks, the surgeon will remove contaminated tissue and close the internal fistula opening.
Options that do not involve surgery include:
- Fibrin glue and collagen plug:The surgeon cleans out the passageway and then sutures the hole to the interior. After that, a fibrin-based special glue is injected via the fistula's exterior opening. Fibrin is a protein that has a fibrous structure. Also, the anal fistula tunnel can be closed after being plugged with a collagen protein plug and subsequently sealed.
- Seton placement:A seton is inserted into the fistula by the surgeon to assist in the drainage of the infection. This enables the tunnel to recuperate. Surgical intervention can be necessary after this operation.
- Medication:If Crohn's disease is the underlying cause of an anal fistula, then the therapy may involve taking medication.
In instances of an anal fistula that is more complex, more extensive surgeries, such as muscle flap and ostomy and soma, may be advised.
What Is an Anal Fistula?
Prevention Of Anal Fistula
You can significantly lower your likelihood of developing an anal fistula if you take steps to prevent constipation, maintain the softness of your stools, and open your intestines as soon as you feel the desire to defecate by going to the bathroom. It is essential to consume a large amount of fluids and engage in frequent physical activity if you want to ensure that your bowels function normally and that your stools remain soft.
People Also Ask
What Happens If Fistula Is Left Untreated?
Fistulas can be very painful, and if they aren't taken care of, they can lead to serious problems. Some fistulas can cause a bacterial infection, which can lead to sepsis, a dangerous condition that can cause low blood pressure, organ damage, or even death.
Can Fistula Be Cured?
For a fistula to heal, tighter setons may be used to slowly cut through it. This may require more than one surgery, which the surgeon can talk to you about. Or, they might suggest doing several fistulotomies, each time carefully opening a small part of the fistula, or a different treatment.
What Causes An Anal Fistula?
An infection that starts in an anal gland is usually what causes an anal fistula. The infection causes an abscess that drains on its own or is drained surgically through the skin next to the anus. Along this drainage path, a tunnel forms under the skin. This tunnel is called a fistula.
Conclusion
Surgery is usually successful in treating an anal fistula. Following the procedure, your surgeon may advise you to take stool softeners or laxatives for a week, as well as provide you instructions on how to perform a sitz bath, which involves soaking the affected area in a warm bath. If the abscess and fistula are treated appropriately and allowed to heal, there is a good chance that they will not recur.

Daniel James
Author
Daniel James is a distinguished gerontologist, author, and professional coach known for his expertise in health and aging.
With degrees from Georgia Tech and UCLA, including a diploma in gerontology from the University of Boston, Daniel brings over 15 years of experience to his work.
His credentials also include a Professional Coaching Certification, enhancing his credibility in personal development and well-being.
In his free time, Daniel is an avid runner and tennis player, passionate about fitness, wellness, and staying active.
His commitment to improving lives through health education and coaching reflects his passion and dedication in both professional and personal endeavors.

Karan Emery
Reviewer
Karan Emery, an accomplished researcher and leader in health sciences, biotechnology, and pharmaceuticals, brings over two decades of experience to the table. Holding a Ph.D. in Pharmaceutical Sciences from Stanford University, Karan's credentials underscore her authority in the field.
With a track record of groundbreaking research and numerous peer-reviewed publications in prestigious journals, Karan's expertise is widely recognized in the scientific community.
Her writing style is characterized by its clarity and meticulous attention to detail, making complex scientific concepts accessible to a broad audience. Apart from her professional endeavors, Karan enjoys cooking, learning about different cultures and languages, watching documentaries, and visiting historical landmarks.
Committed to advancing knowledge and improving health outcomes, Karan Emery continues to make significant contributions to the fields of health, biotechnology, and pharmaceuticals.
Latest Articles
Popular Articles