Microglia Activation - How It Can Better Traumatic Brain Injuries
This article emphasizes the dual-edged sword function of microglia activation, as microglia can be both pro-survival and pro-death in the aftermath of TBI. There have been presented new and current inflammation-based biomarkers for the treatment of TBI, which may promote regenerative capacity and diminish degenerative events connected to microglial response. Microglia provide neuroprotection by phagocytosing improperly penetrated foreign particles and encapsulating them in their own cell bodies.
Author:Katharine TateReviewer:Karan EmeryOct 12, 2022215 Shares2.9K Views
This article emphasizes the dual-edged sword function of microglia activation, as microglia can be both pro-survival and pro-death in the aftermath of TBI.
There have been presented new and current inflammation-based biomarkers for the treatment of TBI, which may promote regenerative capacity and diminish degenerative events connected to microglial response.
Microglia provide neuroprotection by phagocytosing improperly penetrated foreign particles and encapsulating them in their own cell bodies.
Microglial cells' phagocytic capacity also declines with age.
TBI and other comorbidity variables have a tendency to worsen clinical symptoms, making it difficult to develop drugs that target microglial activation.
A traumatic brain injury (TBI) happens when an object penetrates the skull and damages brain tissue following a severe blow, jolt, impact, or jolt to the head.
What Is The Definition Of Microglia?
Microglia cells are central nervous system immune cells that play crucial roles in brain infections and inflammation. Recent in vivo imaging studies have showed that microglia are very dynamic in the resting healthy brain, moving constantly to actively inspect the brain parenchyma.
These active microglia respond quickly to pathogenic stresses, activating to produce a variety of actions that may contribute to pathogenesis or give neuronal protection. Under more normal, physiological conditions, interactions between microglia and neurons are recognized as vital in shaping neuronal circuit activity.
Microglia interactions with neurons during development and neurogenesis contribute to shape the final patterns of neuronal circuits critical for behavior and illness. Microglia in the mature brain can respond to changes in sensory activity and alter neuronal activity both acutely and long-term. Microglia appear to be particularly involved in monitoring synaptic function integrity.
Microglia activation has been found in a variety of CNS illnesses and is critical for organizing immune system resources during disease-associated neuroinflammation. Activated microglia, for example, are the most common phagocytes found in early stage multiple sclerosis (MS) lesions.
This alters as the lesion progresses, with recruited bone marrow-derived macrophages taking over. More information comes from mouse hepatitis virus (MHV) infection, which causes demyelinating illness in experimental autoimmune encephalomyelitis models (EAE).
Microglia boost the expression of cytokines that decrease viral infection and signal to adaptive immune cells shortly after MHV infection.
Meet Your Microglia: Your Brain's Overlooked Superheroes
The Immune System And Microglia
TBI, as well as other neurological illnesses, as well as aging and degenerative diseases such as Alzheimer's and Parkinson's, have been associated to increased immune system activation in the central nervous system (CNS).
A study of microglia phenotypes discovered three distinct types: I resting, ramified microglia; (ii) activated, non-phagocytic [or antigen presenting cell (APC)-like] microglia in areas of CNS inflammation; and (iii) reactive microglia, which include phagocytic microglia in response to injury or infection (based on developmental and pathophysiologic studies).
Depending on their level of activation, macrophages and microglia can polarize into two major subtypes, M1 and M2.
The M1 subtype's overproduction of proinflammatory cytokines boosts cell-mediated immunity. This condition is characterized by high levels of interferon-gamma (IFN-γ), tumor necrosis factor (TNF-α), interleukin-1, IL-12, and low levels of IL-10.
When microglia come into contact with HIV proteins, they may develop the M1 phenotype (such as transactivators of transcription [Tat] bind toll-like receptors 3 or 4 as well). M2 microglia produce anti-inflammatory IL-10 and TGF-β, as well as cytokine signaling repressors, which reduce inflammation and clean up cellular waste (including amyloid plaques) (SOCS).
They are both microglial phenotypes of type ii or iii. The factors that induce polarization to M1 or M2 reinforce a cycle-like phenotype.
Following a TBI, the early inflammatory response causes neuronal damage and disruption of the blood-brain barrier. Microglial cells become activated in minutes and operate as APCs, releasing proinflammatory cytokines and chemokines, similar to peripheral macrophages.
Following injury, activated microglia produce additional neurotoxic products like as nitric oxide (NO) and superoxide free radicals, which generate reactive oxygen species (ROS) and reactive nitrogen species (RNS) (RNS).
Microglial cells stay activated for at least a year in animal models of cortical controlled impact (CCI), fluid percussion brain damage in rats, and combined unilateral lesion of the primary motor cortex and lateral premotor cortex in rhesus monkeys.
Human postmortem studies have revealed microglial activity in subcortical brain locations 17 years after TBI. These findings point to the persistence of a persistent inflammatory state mediated by microglia.
Utilization Of Microglial Survival Functions
Strategies that target specific molecules may be used to modify the cytokine profile of activated microglia. Using a variety of substances, it is possible to promote the survival of neurons after injury.
Microglia can be stimulated in vitro by granulocyte-macrophage colony stimulating factor (GM-CSF) and colony stimulating factor 1 (CSF-1). In response to adequate signaling signals, microglia may begin producing neuroprotective molecules (including IL-10, IL-1ra, and TGF-β) shortly after injury.
Proinflammatory cytokines are immediately decreased as a direct result of these drugs. TGF-β has been related to neuroprotective features such as improved function, reduced lesion size, and decreased iNOS formation following injury.
Potential activated microglia-related biomarkers should have the following characteristics:
- High specificity and sensitivity for activated microglia
- Stimulate microglia to polarize into the M2 phenotype
- Promote synaptic, neuronal plasticity, and cell survival at a close or distal range from the site of injury
- Reduce the inflammatory response post-TBI. The chemokine fractalkine, CX3CL1, and its receptor CX3CR1 may be potential microglia-related indicators to which the above criteria might be applied to drive microglia into the M2 phenotype. Both are expressed constitutively in the neurological system. The ligand is only found in neurons and endothelial cells, but the receptor is found in microglia, astrocytes, and neurons. CX3CL1 lowers microglia toxicity and, as a result, neuronal damage in in vitro and in vivo models of neurological disorders and brain inflammation.
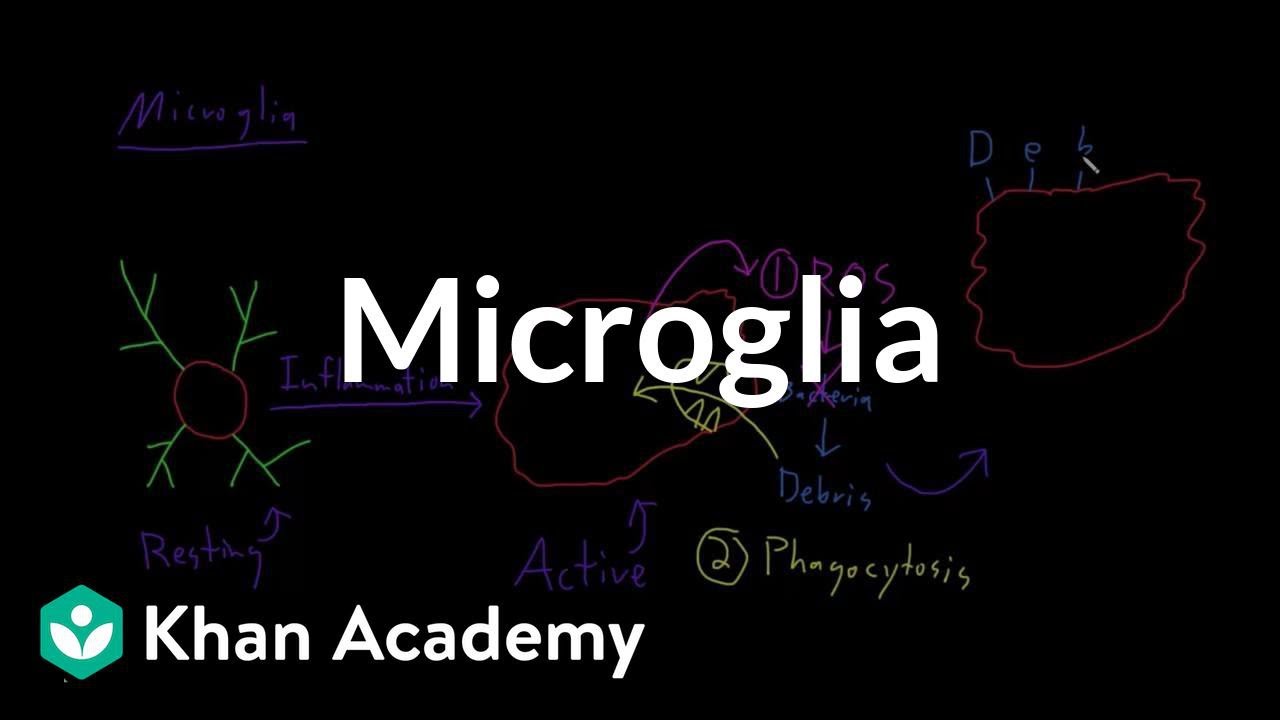
Microglia | Nervous system physiology | NCLEX-RN | Khan Academy
Increasing Microglial Phagocytic Activity
The phagocytic function of microglia, which may prevent neurodegeneration, is also appealing. Microglial phagocytic activity early after TBI may limit the spread of cell death signals to wounded neurons and other surrounding cells.
Furthermore, multiple investigations have demonstrated that cell autophagy is neuroprotective after a traumatic brain injury (TBI). Neighboring neurons and astrocytes can clear cell debris from the afflicted area after a brain injury.
Researchers discovered an increase in autophagosomal formation proteins, such as microtubule-associated protein 1 light chain 3 (LC3) and beclin 1, in neurons and astrocytes following TBI at 1-h, 3-h, and 32 days.
This could be because autophagy eliminates healthy cells alongside damaged ones, thereby exacerbating TBI symptoms. To delay the progression of TBI pathology while limiting its negative side effects, microglia phagocytic activity must be managed.
Redirecting Microglial Death-Promoting Functions
Inactivating the pro-death inflammatory response of microglial cells is similarly efficient in preventing TBI-associated secondary cell death. Recent pharmaceutical approaches to TBI-induced secondary cell death use oxidative stress and microglial activation inhibitors.
Apocynin, a NADPH oxidase assembly inhibitor that retains the proinflammatory character of microglia, has therapeutic promise in mouse models of TBI at a high dose (100 mg/kg). One week after TBI, microglial activation persisted, but apocynin suppressed ROS production in hippocampal CA3 pyramidal neurons; they also discovered reduced BBB disruption and neuronal rescue from TBI-induced cell death.
New therapeutics to reduce microglia activation have emerged as a result of research into possible biomarkers identified in models of acute spinal cord injury (SCI).
Interestingly, an overlap in the cytokine profiles expressed by SCI rats and human individuals has recently been revealed, in that rodents and people released IL-6, IL-8, and monocyte chemoattractant protein 1 in a SCI injury-dependent way (MCP-1). The antibiotic minocycline is a promising neuroprotective strategy.
Minocycline has been demonstrated to reduce microglial activation, excitotoxicity, and neuronal and oligodendrocyte cell death associated with mitochondrial stabilization in SCI animal models.
Considering Biomarkers Based On Microglia For TBI
Researchers should devote their time and resources to discovering TBI biomarkers, which will aid in the development of TBI treatments, because the timing of treatment will be governed by secondary cell death as detected by novel biomarker technologies.
Cytokine Profiling
The identification of specific proteins that regulate microglia (e.g., BDNF) via cytokine profiling of microglial cells may provide information about the TBI patient's state by identifying these proteins in the blood or CSF.
Unraveling the cytokine and chemokine profiles of proteins that influence microglia response to TBI could lead to the discovery of previously undiscovered cytokines and chemokines in activated microglia. This strategy must address paracrine and autocrine processes, as well as cytokines, chemokines, and neurotrophic/tropic chemicals.
The cytokine profile of TBI-induced activated microglia could provide new insights into previously employed neuroprotective methods. Measurements of these well-known proteins in blood, plasma, or cerebral spinal fluid (CSF) may be utilized in human clinical settings to offer information on the health of TBI patients.
A bedside monitor, such as cerebral microdialysis, can provide real-time evaluation of brain tissue biochemistry in neurointensive care.
If future study uncovers an overlap between the microglial cytokine profile and the microdialysis data processing, it may be viable to use brain tissue microdialysis to monitor acute and chronic TBI.
Tyrosine kinase, poly(ADP-ribose) polymerase-1, and primary myeloid differentiation response protein 88 are biomarkers identified in rat models of TBI that should be included in microglial profiling and whole brain tissue profiling by microdialysis (PMP88).
Aside from this emerging cytokine profile, high-throughput screening procedures (e.g., microRNA analysis) using blood, CSF, or tissue samples from TBI patients and animal models may identify additional cytokines and associated proteins.
Detecting Profile Of Phagocytosis
The phagocytic characteristic of microglia may emphasize the close molecular and biological relationship between NPCs and stem cells. Imaging methods like as functional MRI can also be used to assess microglia phagocytic activity.
Microglia, NPCs, and stem cells all have phagocytic profiles that may disclose immunomodulatory proteins, which could help us understand how the modulatory and phagocytic activities of different cell types intersect. Imaging methods (for example, functional MRI) can be utilized to track NPC or stem cell levels in order to provide a real-time status of microglia phagocytic activity.
As an alternative, we may try to connect known phagocytic indicators (such as LC3) to apoptosis and inflammatory markers in the TBI brain to see whether there is a link between the three. Following lateral mild fluid percussion damage in adult rats, time-dependent gene expression variations in 23 apoptosis-related genes, including IL-1-α, IL-1-β, and TNF, which elevated swiftly at 3 hours after the injury, were discovered.
As a result, these time-dependent gene expression patterns shed information on the progression of apoptosis, which was connected to inflammation in this investigation.
Assessing The Level Of Microglial Proinflammatory Response
The degree of "proinflammatory response of microglia" might be determined using blood/CSF tests. The image below depicts pro-inflammation that is therapeutic (i.e., acting as a signaling cue for stem cell migration from the periphery to the brain) but has not yet reached a threshold that may initiate the neuroinflammatory response responsible for aggravating TBI clinical symptoms.
If S-nitrosoglutathione (GSNO) levels are tested, it may reveal brain levels of peroxynitrite and oxidative metabolites, which when lowered may indicate that the neurovascular unit integrity is being protected. Long-term GSNO therapy at low levels may promote synaptic plasticity by increasing neurotrophic factors.
In order to better understand how TBI impacts neurovascular health and synaptic plasticity in the brain, peroxynitrite and other reactive oxygen species, as well as neurotrophic factors, can be employed as surrogate markers of GSNO.
People Also Ask
What Cytokines Causes Microglia Activation?
Microglia are activated in the CNS in response to a variety of pathological conditions such as damage, ischemia, and infection. When microglia are activated, they produce pro-inflammatory cytokines such as IL-1, IL-6, and TNF-α.
Can Sodium Ions Cause Microglia Activation?
Six sodium channels play a role in the activation and functional regulation of microglia in EAE and MS, suggesting that they could be used as a therapeutic target.
What Is Microglia Activation And Inflammation?
Microglial activation is in charge of immunological surveillance in the CNS. When exposed to noxious stimuli, they respond by producing inflammatory mediators and mounting an effective inflammatory response. Following this, anti-inflammatory mediators are released, and the inflammatory reaction is resolved.
What Happens If Microglia Are Damaged?
However, if the inflammation persists for an extended period of time, the process can begin to kill healthy brain cells. Uncontrolled inflammation in the brain induced by microglia has been linked to neurodegenerative disorders such as Alzheimer's, Parkinson's, and Amyotrophic Lateral Sclerosis.
Conclusion
Phagocytic activity of microglia activation is an important survival characteristic. Identification of the signaling pathways that foster microglia to preserve their regenerative function after injury, rather than the predominating inflammatory activity, would provide insights into homeostatic processes for maintaining a healthy brain (e.g. neuroinflammation).
The ability of microglia to migrate to the site of injury is an intriguing property that warrants more investigation. Little is known, however, regarding the migratory processes that thriving microglia use to colonize the CNS once they reach the injured brain.
The study of the molecular signals that drive the anti-inflammatory response will lead to the development of effective treatments to mitigate the negative consequences of microglial activation and redirect their function toward microglia-based medicines for TBI.

Katharine Tate
Author

Karan Emery
Reviewer
Latest Articles
Popular Articles